Gout, Rheumatoid arthritis, and Osteoarthritis -- Causes and Treatment
Gout, rheumatoid arthritis, and osteoarthritis are three distinct medical conditions, each with its own set of causes.
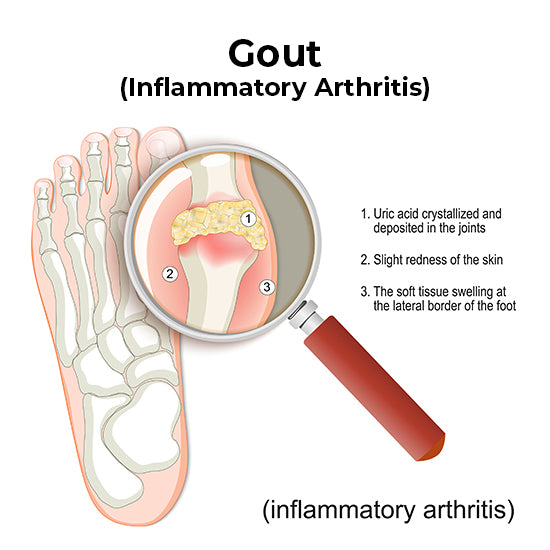
Gout is a type of arthritis caused by the buildup of uric acid crystals in the joints. This occurs when the body produces too much uric acid or when it cannot effectively eliminate it through urine. Factors such as diet, genetics, obesity, and certain medications can contribute to the development of gout.
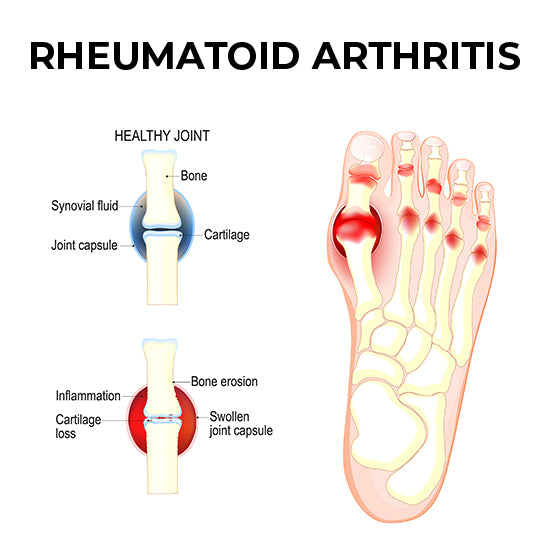
Rheumatoid arthritis, on the other hand, is an autoimmune disorder in which the body's immune system mistakenly attacks the synovium—(the lining of the membranes that surround the joints. The exact cause of rheumatoid arthritis is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental triggers, such as infections or exposure to certain toxins.
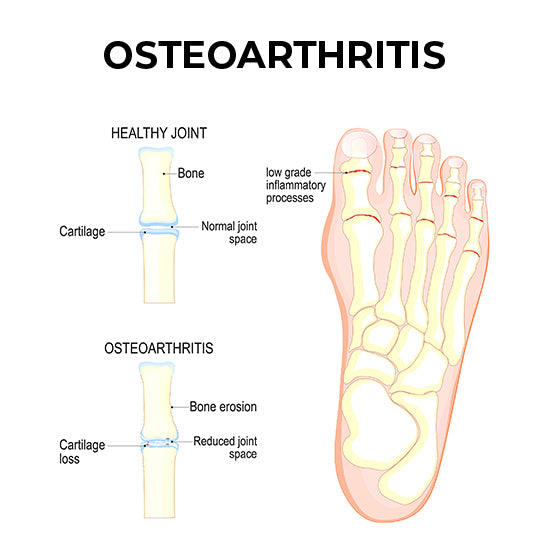
Osteoarthritis is primarily a degenerative joint disease that occurs when the protective cartilage that cushions the ends of bones wears down over time. While age is a significant risk factor, other causes of osteoarthritis include joint injuries, obesity, genetics, and joint overuse or misuse.
Tips for Treatment:
Treatment options for gout, rheumatoid arthritis, and osteoarthritis can vary significantly, and the choice of footwear and orthotics play an important role in managing these conditions.
- Gout: Proper footwear for gout patients should prioritize comfort and support. Choosing shoes with cushioned soles and a wide toe box can help reduce pressure on affected joints. Custom orthotic insoles may be recommended to provide additional arch support and shock absorption. Avoiding tight-fitting or high-heeled shoes is crucial, as they can exacerbate symptoms during gout flares.
- Rheumatoid Arthritis (RA): In the case of RA, footwear needs to accommodate joint deformities and provide stability. Shoes with adjustable straps or laces can ensure a secure fit. Orthotics can be custom-designed to align the foot and reduce pressure on specific joints affected by RA. Additionally, cushioning and shock-absorbing materials in the sole can help minimize discomfort during walking.
- Osteoarthritis (OA): Footwear for OA should prioritize stability and shock absorption. Shoes with a low, wide heel and good arch support can help distribute weight evenly, reducing stress on affected joints. Custom-made orthotics can be beneficial to individuals with OA because they can be tailored to provide the necessary support and alignment for their unique foot anatomy.
In all cases, it's essential to consult with a healthcare professional or a podiatrist who specializes in managing arthritis-related foot problems. They can assess your specific condition, recommend suitable footwear options, and provide guidance on orthotics or other assistive devices to help you maintain mobility and alleviate discomfort associated with gout, rheumatoid arthritis, or osteoarthritis. Properly chosen shoes and orthotics can significantly contribute to the overall management and quality of life for individuals living with these conditions.
*We are not doctors, and the information provided here is only meant for informational purposes, not diagnosis. If you suspect you have a foot condition, please talk to your doctor so they can discuss the best solution for you.




